Key Takeaways:
- Legacy medical devices running old code create growing cybersecurity and patient safety risks
- Ransomware attacks on hospitals show how downtime directly impacts clinical care
- Security transparency and SBOMs are now key to winning healthcare procurement deals
- Cyber resilience—not just compliance—will define the next era of connected healthcare
Hospitals and medical device manufacturers are facing a quiet crisis rooted not in cutting-edge exploits or nation-state hackers, but in old software.
Across healthcare, legacy code is turning routine cybersecurity weaknesses into real-world patient safety risks. The problem is simple to explain and hard to solve: devices built to last for decades are now connected to modern networks, yet run on outdated and difficult-to-patch code.
As connected devices become the norm, this technical debt has become a liability that extends to patient care.
In a discussion on the business realities of medical device cybersecurity, Shane Fry, CTO of RunSafe Security, Patrick Garrity, Security Researcher at VulnCheck, and Phil Englert, VP of Medical Device Security Health-ISAC, discussed the vulnerability and compliance landscape and where software security comes into play.
Watch the full webinar for more on medical device cybersecurity here.
When “Forever Devices” Become Forever Vulnerable
A medical device can remain in use for 15-20 years. That longevity might make sense for hospitals managing costs, but it means the software inside those devices is often frozen in time. Meanwhile, the threat landscape moves forward.
“These devices can be used for decades,” said Patrick Garrity, Security Researcher at VulnCheck. “That becomes a real challenge. Manufacturers have to be mindful of that.”
Imagine a connected infusion pump or imaging system that still relies on a Windows 7 or even XP base. Patches stop, drivers go unsupported, and over time, the device becomes a soft target on an otherwise modern network.
And because medical systems are tightly integrated—feeding data into hospital EMRs, remote dashboards, and cloud platforms—an outdated component in one corner of the network can expose an entire healthcare operation.
When Cyber Weaknesses Become a Patient Safety Risk
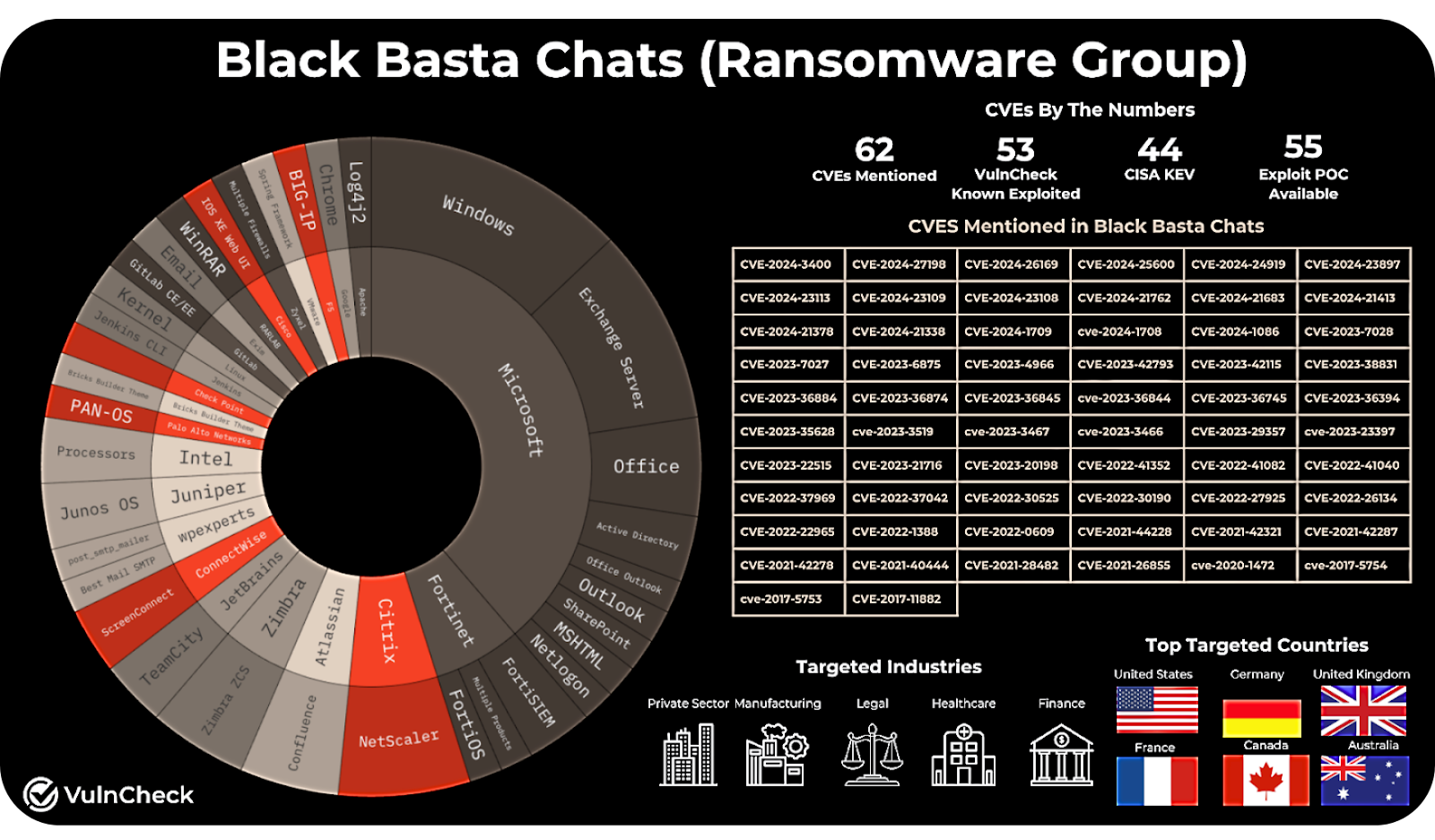
The stakes became clear during the Black Basta ransomware attack on Ascension Health earlier this year. Hospitals were forced to revert to paper-based systems. Electronic medical records, scheduling systems, and digital imaging were suddenly inaccessible.
RunSafe Security CTO Shane Fry summed up the real-world impact: “If your network’s down, you can’t do surgery.”
Beyond the immediate operational disruption, the consequences for patients were serious. Doctors faced delays accessing treatment histories. Pharmacists couldn’t verify prescriptions electronically. In some facilities, even infusion pumps and lab equipment had to be taken offline as a precaution.
Ransomware may be the headline, but the underlying vulnerability is the same—cybersecurity weaknesses left unaddressed.
As Phil Englert, VP of Medical Device Security at Health-ISAC, noted: “Cyber is a failure mode. It’s a way for things not to work or not to work as intended when you want them to.”
When software failures and weak security controls ripple into care delivery, cybersecurity is a patient safety imperative.
Where Exploitation Starts
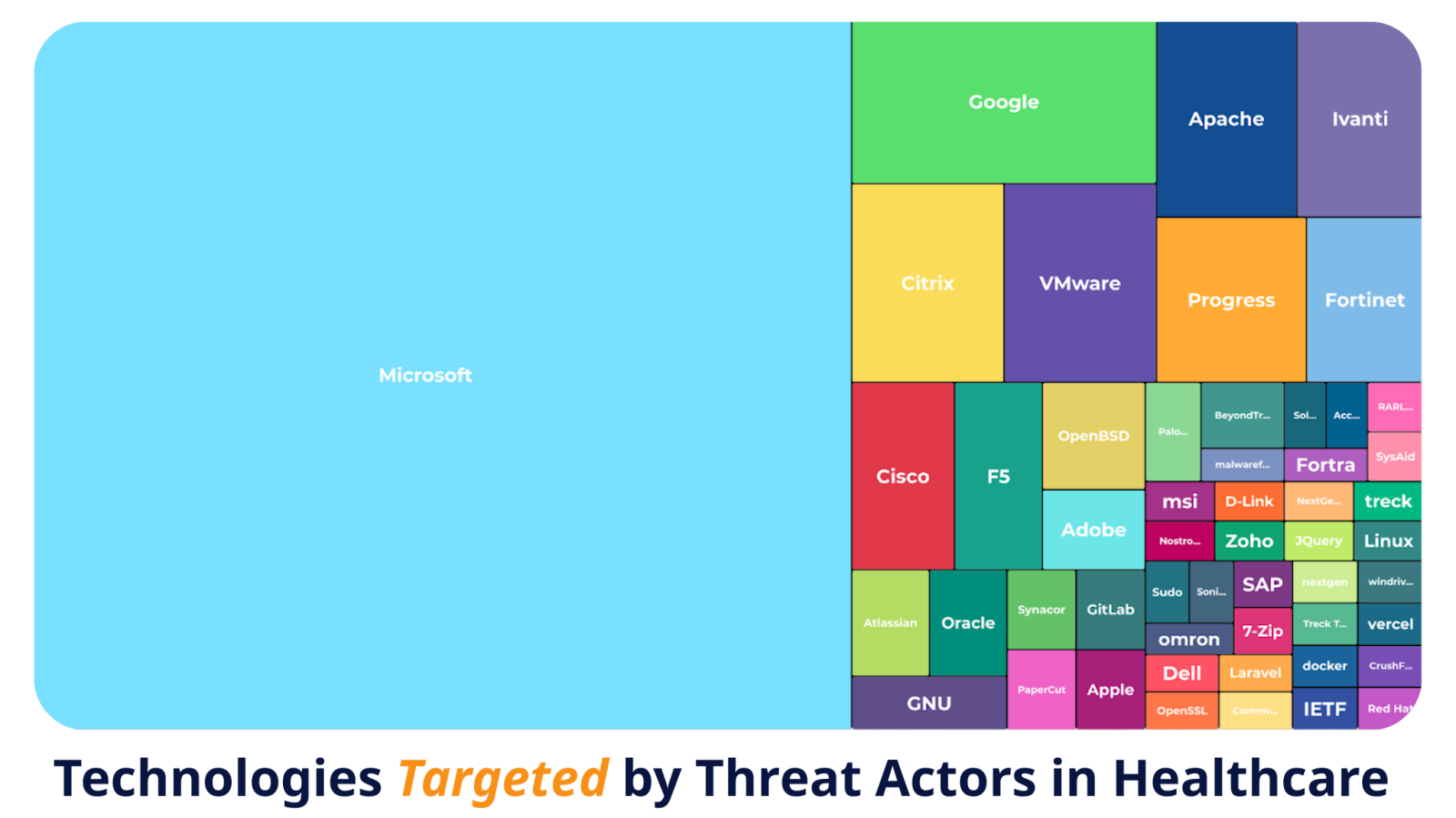
Most healthcare breaches don’t start with exotic zero-days. They start with vulnerabilities everyone already knows about.
Attackers target what’s common: outdated Microsoft servers, unpatched remote access tools, misconfigured network gateways, and open-source components left to age quietly inside medical devices.
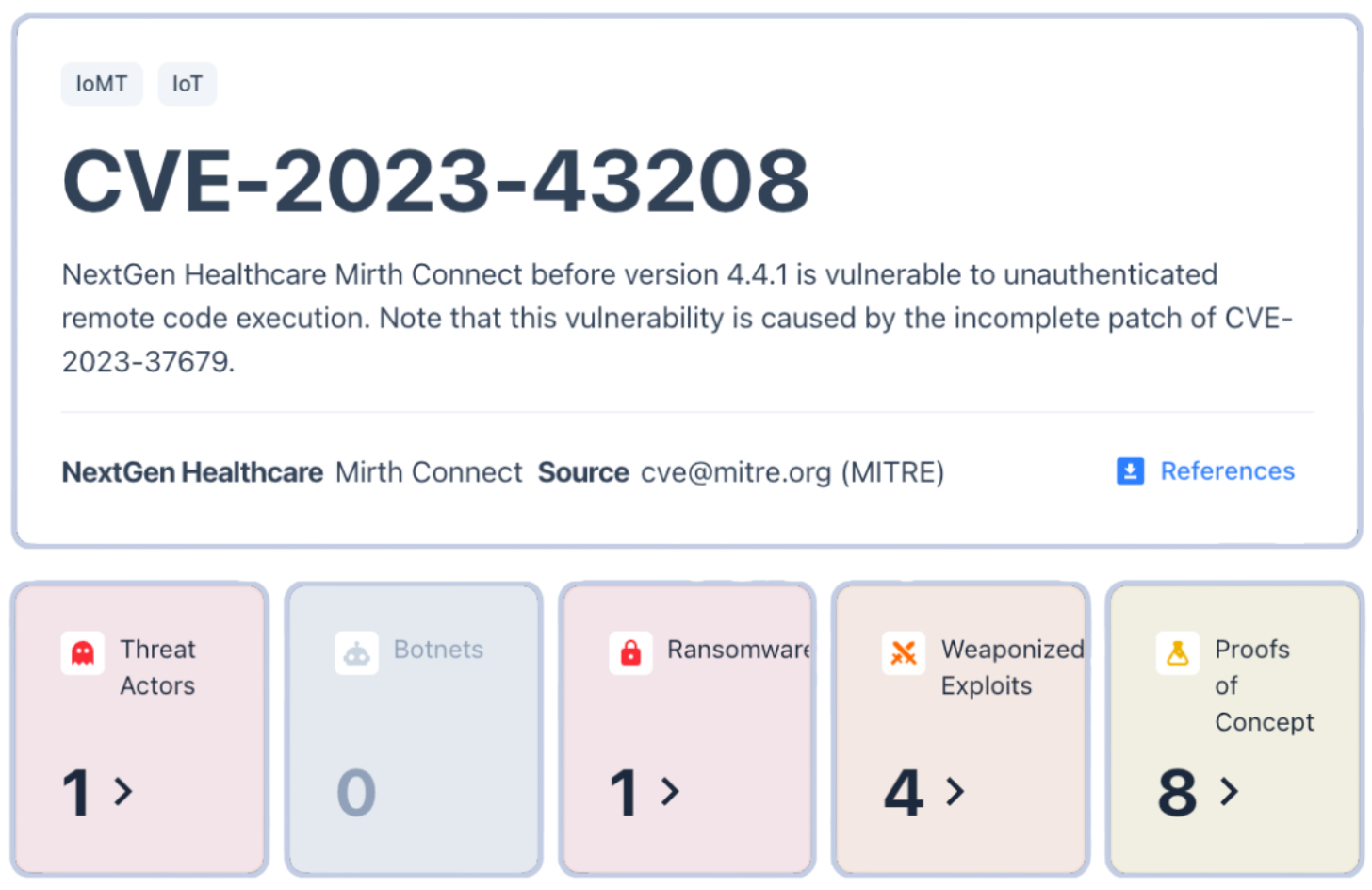
Garrity pointed to examples such as NextGen Healthcare’s Mirth Connect, a popular data exchange system exploited in ransomware campaigns. The flaw wasn’t obscure, as it had been publicly documented and patched. Yet more than a year later, vulnerable systems remained exposed online, still running unpatched versions.
“Threat actors are going to opportunistically target anything and everything. And… they’re just using what’s already published and off-the-shelf,” Garrity said. “Even outdated remote management tools or cloud connectors can become attack surfaces.”
Legacy software turns these well-known weaknesses into long-term liabilities. Once a system goes unpatched, every new connection—every piece of cloud integration or remote monitoring—adds to the risk.
The Business Risk of Standing Still
The consequences of cybersecurity weaknesses aren’t limited to downtime or headlines—they directly affect revenue and market access.
According to RunSafe Security’s 2025 Medical Device Cybersecurity Index, 83% of healthcare buyers now include cybersecurity standards in their RFPs, and 46% have declined to purchase medical devices due to security concerns. Outdated or insecure software doesn’t just pose a technical problem; it can cost sales.
For device manufacturers, the message from buyers is unmistakable: security maturity equals market readiness. Procurement teams are treating cybersecurity posture as a business criterion alongside clinical performance and cost.
Hospitals, too, are taking notice. Many are implementing procurement checklists requiring vendors to provide Software Bills of Materials (SBOMs), vulnerability response plans, and clear lifecycle support documentation. Without those, even innovative technologies struggle to clear the contracting stage.
Modernizing Security for Long Device Lifespans
Managing legacy code in a regulated, high-stakes industry isn’t easy, but it’s not impossible. The most resilient organizations are taking pragmatic, layered steps to reduce risk without overhauling every device.
1. Build-Time SBOMs
Create and maintain Software Bills of Materials (SBOMs) during the build process, not after. This ensures visibility into every dependency and allows for continuous monitoring of vulnerabilities over time.
2. Exploit-Based Prioritization
Focus patching on vulnerabilities with known exploitation in the wild, not just those with high CVSS scores.
3. Compensating Controls
Where patches aren’t possible, use segmentation, strict access controls, and runtime protections to reduce exposure.
4. Design for the Next Decade
Reserve processing and storage capacity for future updates and plan for cryptographic agility so devices remain secure over their full lifespan.
5. Transparent End-of-Life Policies
Communicate openly about support timelines and risk mitigation options. Buyers and regulators increasingly view transparency as part of good cybersecurity hygiene.
From Compliance to Resilience
Healthcare is shifting from a “check-the-box” approach to one centered on resilience. Regulators are reinforcing that shift: the FDA’s premarket guidance now requires SBOMs and vulnerability management plans, while the EU’s Cyber Resilience Act pushes similar expectations globally.
The result is a new baseline where cyber hygiene and secure design aren’t just best practices, they’re business necessities.
“If you don’t know what’s in the software you’re deploying to your networks, then how can you know that a vulnerability affects you?” Fry said. “Without that Software Bill of Materials, you’re going to be very limited.”
For manufacturers and healthcare providers alike, addressing legacy code is about security and trust. It’s about maintaining operational continuity. And ultimately, it’s about keeping patients safe in a world where every connected device is part of the care equation.
As Fry put it: “Everything that we should be doing in cybersecurity should be viewed through … the lens of making sure the patient can get the best care they need as quickly as they can.”
For more on medical device challenges and defenses, listen to our panel discussion: From Ransomware to Regulation: The New Business Reality for Medical Device Cybersecurity.